
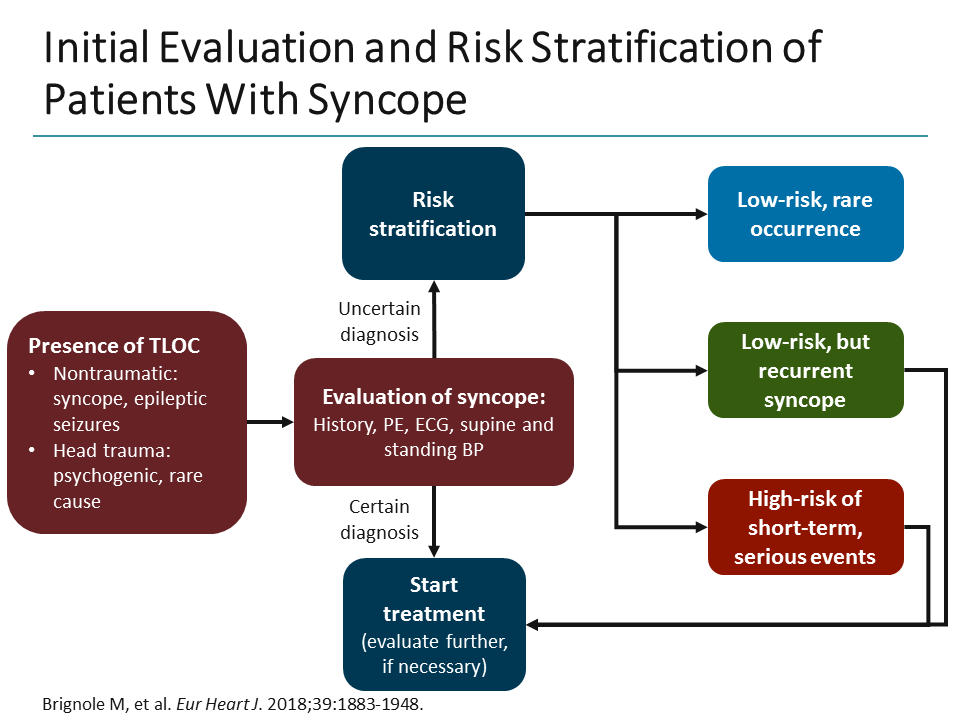
Patients can be reassured that, in the absence of underlying cardiac disease, syncope itself is not associated with increased mortality.Even inpatient telemetry, a routine part of standard evaluation, is helpful only 5% of the time. Cardiac enzymes, electroencephalography, CT scan of the head, and carotid ultrasonography contribute to diagnosis in less than 1% of cases.Initial evaluation of syncope should include medical history, physical examination, ECG, and postural blood-pressure testing.Among diagnostic tests, orthostatic blood pressure measurement (performed in about one-third of cases) is both the highest-yield test and the least expensive.An estimated 86% of individuals seen in the ED after a syncopal episode are admitted to the hospital.3 True syncope can be associated with other concerning causes, such as aortic stenosis, aortic dissection, and massive pulmonary embolus, as well as arrhythmias from underlying cardiac disease. 2 The primary objective for evaluation is identification of individuals at increased risk of death due to associated conditions, especially cardiac conditions such as structural heart disease myocardial ischemia and infarction (MI) Wolff-Parkinson-White, Brugada, or long QT syndromes and polymorphic ventricular tachycardia. Syncope is a common problem, accounting for 1% to 2% of ED visits in the U.S. Nonsyncopal mechanisms, such as seizure and hypoglycemia, should also be considered in the differential diagnosis of transient loss of consciousness (see Table 1, p. The differential diagnosis of syncopal loss of consciousness includes neurally mediated (e.g., vasovagal) syncope, orthostatic hypotension, cardiac arrhythmias, structural heart disease, and cerebrovascular disease.Īmong young, otherwise healthy people, neurally mediated syncope, which has a relatively benign prognosis, is by far the most common etiology, while in older patients, primary cardiac causes are more common. The final common pathway of all causes of syncope is global cerebral hypoperfusion-specifically, hypoperfusion of the reticular activating system. Syncope is defined as sudden, self-terminating loss of consciousness. What is the most cost-effective evaluation for this patient admitted with suspected first syncopal episode? The primary E&M objective is identifying patients at increased risk of death due to associated conditions (e.g., heart disease, myocardial ischemia). Insertion of a pacemaker is the standard treatment for syncope caused by a slow heartbeat (bradycardia).Syncope accounts for 1% to 2% of ED visits in the U.S.Simple reassurance, proper hydration, anticipatory guidance, safety precautions, and increased salt intake are helpful for common type fainting (vasovagal syncope) especially in children and young adults.When you stand up, gravity causes blood to settle in the lower part of your body, below your diaphragm. It is caused by a sudden drop in blood pressure, which causes a drop in blood flow to the brain. Vasovagal syncope is the most common type of syncope. The type you have depends on what causes the problem. Still, syncope is always a potentially serious issue, both because it may indicate a serious underlying problem, and because any loss of consciousness can produce injury.Īlso question is, what is the most common cause of syncope? abrupt changes in posture, such as standing up too quickly, which can cause blood to pool in the feet or legs.įurthermore, is near syncope serious? Syncope (sin-co-pee) is a temporary loss of consciousness, commonly referred to as fainting, or passing out.low blood pressure or dilated blood vessels.Each time you have this feeling is called a near syncope episode. What is near syncope? Near syncope, also called presyncope, is the feeling that you may faint (lose consciousness), but you do not.


 0 kommentar(er)
0 kommentar(er)
